7 Risk factors for autoimmune disease
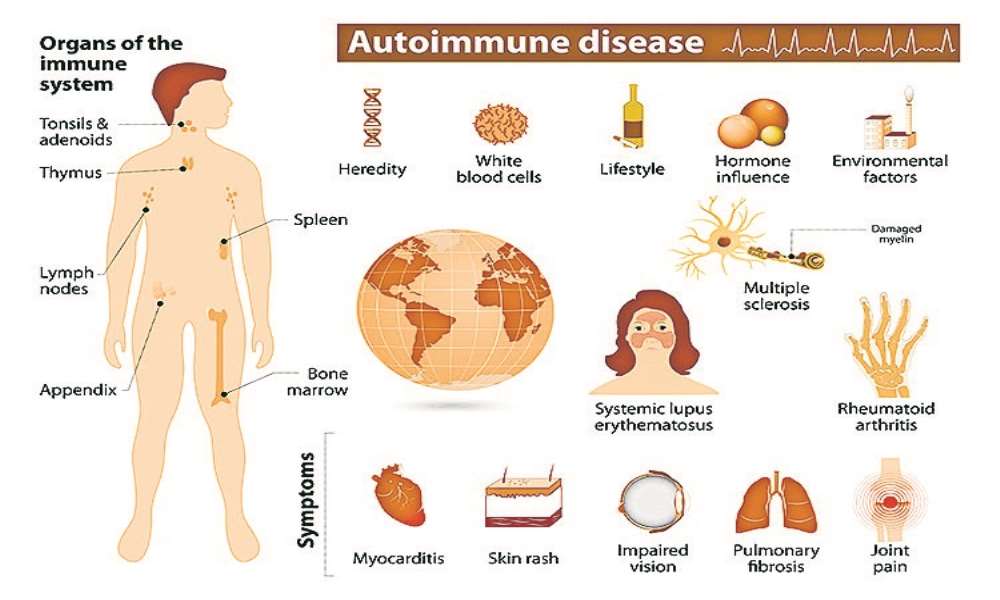
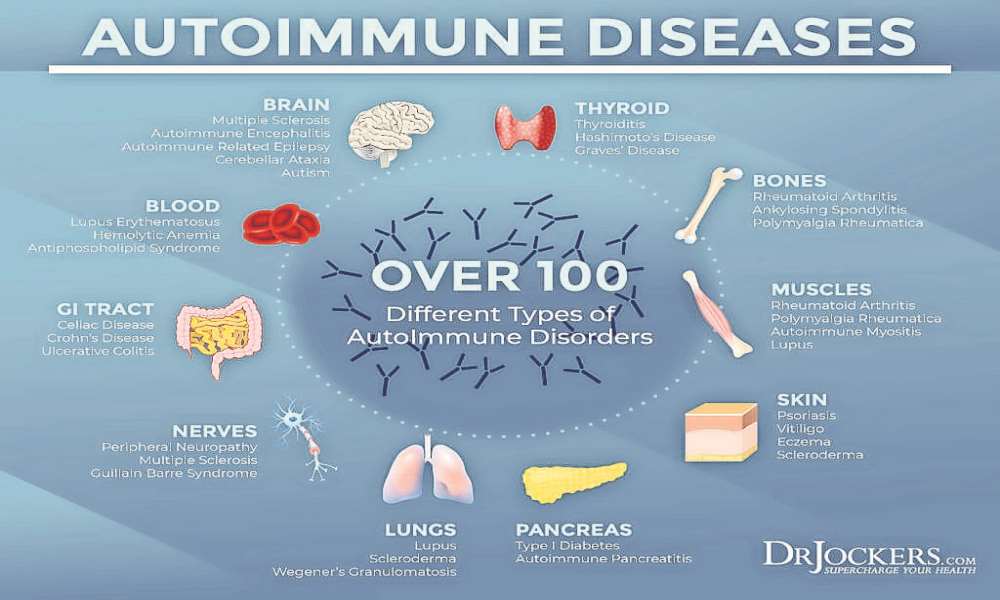
While researchers are still digging for answers on exactly what causes over 80 autoimmune diseases, there are certain risk factors that are believed to impact immune tolerance and may lead to the development of autoimmune conditions.
Keep in mind that while falling into one or more of these categories may increase your susceptibility, it does not mean you’re destined to develop a disorder.
1. YOUR SEX
Overall, 78% of people affected by autoimmune disease are female. Regarding specific conditions, up to 95% of systemic lupus erythematosus (SLE) and Sjogren’s syndrome patients are female. Other conditions like arthritis and multiple sclerosis (MS) occur in females around 60% more than in males.
Factors that differ between sexes like the additional X chromosome, certain hormonal changes, reproductive function, immune responses, effects of environmental agents, and organ vulnerability could all have a hand in the higher autoimmune disease prevalence in females.
2. GENETICS
Certain disorders, such as lupus and multiple sclerosis, tend to run in families. If you have relatives with autoimmune disease, then you are more likely to develop a condition yourself (though not necessarily the same one).
Having a genetic predisposition towards autoimmunity means that your risk is higher due to an inherited genetic variation – one that may impact immune response. The way that particular gene is expressed can be altered via the epigenome – a layer of chemical tags that sits on top of your DNA.
When environmental triggers – such as toxic chemicals, infections or other physical traumas, intestinal dysbiosis, or dietary factors– interact with the epigenome, they have the ability to activate or deactivate parts of the genome through complex chemical reactions.
Further study on the epigenome is needed, however the field of epigenetics highlights the critical role our lifestyle plays in either generating or preventing disease.
3. HAVING AN AUTOIMMUNE DISEASE
When you already exhibit one autoimmune disease, you’re at risk to develop more.
An accumulation of three or more autoimmune conditions is called Multiple Autoimmune Syndrome (MAS), which is seen in roughly 25% of patients.
It is common for individuals with certain conditions like celiac disease, rheumatoid arthritis, multiple sclerosis, Hashimoto’s, or Sjogren’s to exhibit MAS. The reason is unknown, but it is likely due to a combination of genetics and environmental factors.
4. OBESITY
Given that roughly 35% of the global population and 72% of adults in the U.S. are overweight or obese, it is critical that we recognize the relationship between obesity and other chronic conditions like autoimmune disease.
Excess weight is associated with over ten autoimmune diseases and may be implicated in others. It has been found to increase the risk of developing autoimmune conditions like rheumatoid and psoriatic arthritis.
Fat – or adipose tissue – is involved in many physiological functions, including metabolism and immune system response. When adipose tissue accumulates and becomes dysfunctional, it can lead to increased or dysregulated secretion of compounds called adipokines. In this case, these bioactive substances tend to be pro-inflammatory and significantly alter immune system function.
In other words, obesity sends the body into a chronic state of low-grade inflammation and can threaten an otherwise healthy immune response.
Research in this area is ongoing, but we are discovering that these factors (and potentially others, like alteration of the gut microbiota and intestinal dysbiosis) can lead to organ damage, metabolic syndrome, and autoimmune conditions.
5. SMOKING AND EXPOSURE TO TOXIC AGENTS
It is widely known that smoking cigarettes is not a healthy practice and can lead to cancer. Now, researchers are discovering that smoking is a risk factor in more than just respiratory conditions.
Smoking has been linked to rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, and other autoimmune diseases.
Why? When you burn tobacco, thousands of chemicals are produced – some of which are known to be toxic. Inhaling that smoke impacts the immune system through various complex interactions, including inflammatory responses, immune suppression, dysregulation of cytokines (signaling molecules involved in autoimmunity), and the development of autoantibodies.
Exposure to other toxins like air pollutants, crystalline silica, ultraviolet radiation, or organic solvents are also associated with the development of autoimmune diseases like multiple sclerosis.
Moreover, a genetic predisposition to autoimmunity further increases your risk. Many toxic agents have the ability to alter gene expression. In a nutshell, they can activate an otherwise repressed gene or deactivate an active one, leading to disease.
6. CERTAIN MEDICATIONS
Many people take pharmaceuticals on a daily basis to decrease blood pressure, manage depression and anxiety, or balance cholesterol levels. And it’s common knowledge that these drugs have potential side effects.
We’re discovering that in some cases, these side effects involve immune system function, and will trigger autoimmune reactions.
Certain blood pressure medications, statins, and antibiotics can trigger drug-induced autoimmune conditions like lupus or autoimmune hepatitis.
7. INFECTIONS
Early exposure to certain infections increases your susceptibility to autoimmune disease.
The presence of Epstein Barr Virus (EBV), which tends to present as a mild illness in childhood and then turn dormant, is associated with systemic lupus erythematosus, rheumatoid arthritis, and Sjogren’s syndrome.
Another infectious microorganism – a bacteria called Group A Streptococcus – can trigger heart, joint, and brain-related autoimmune disease including acute rheumatic fever and rheumatic heart disease.
These viruses interact with your genetics through a variety of mechanisms. In short, they can turn on certain genes that impact the immune system’s ability to differentiate between self and non-self, triggering an autoimmune reaction.
SARS-CoV-2 virus is associated with autoimmune disease in various ways, although researchers are still investigating the relationship. COVID-19 infection has been reported to trigger cases of Guillain-Barre syndrome, antiphospholipid syndrome, lupus, and other diseases. - Source: medicalnewsdaily.com
STATS:
Common autoimmune disease testing:
• Antinuclear antibodies (ANA)
• Autoantibodies
• Secretory IgA antibodies
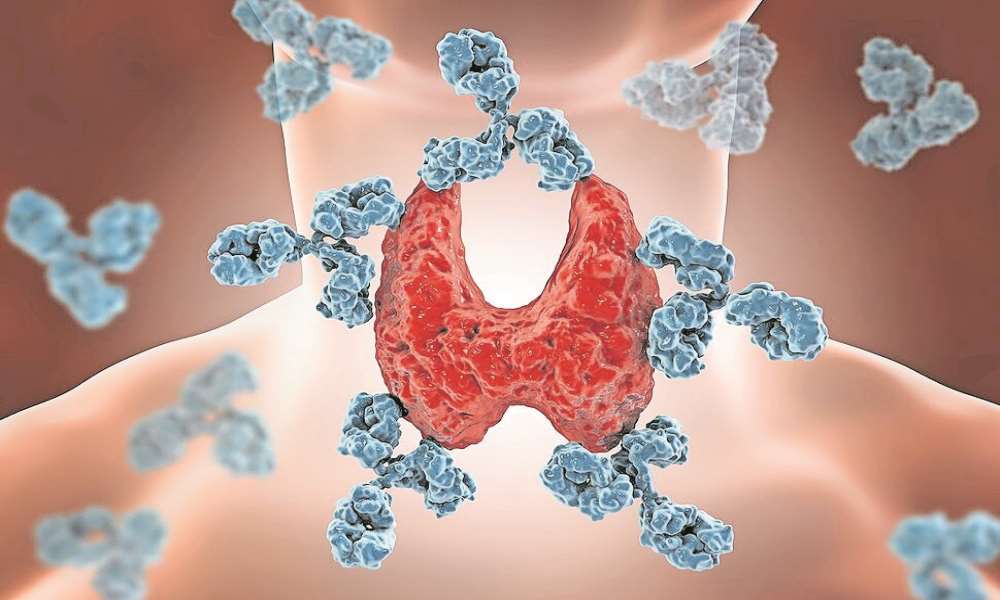
• Thyroid function
• Inflammation
• Organ function
Did you know?
Covid-19
Infectious microorganisms such as SARS-CoV-2 can turn on certain genes and impact the immune system’s ability to differentiate between self and non-self, thus triggering an autoimmune reaction.
Health tip
Eat a nutrient-dense diet and limit processed foods
Health precaution tip
Keep up with the latest information about your medications
Talk with your doctor about specific ways you can reduce your personal risk.
1. YOUR SEX
Overall, 78% of people affected by autoimmune disease are female. Regarding specific conditions, up to 95% of systemic lupus erythematosus (SLE) and Sjogren’s syndrome patients are female. Other conditions like arthritis and multiple sclerosis (MS) occur in females around 60% more than in males.
Factors that differ between sexes like the additional X chromosome, certain hormonal changes, reproductive function, immune responses, effects of environmental agents, and organ vulnerability could all have a hand in the higher autoimmune disease prevalence in females.
2. GENETICS
Certain disorders, such as lupus and multiple sclerosis, tend to run in families. If you have relatives with autoimmune disease, then you are more likely to develop a condition yourself (though not necessarily the same one).
Having a genetic predisposition towards autoimmunity means that your risk is higher due to an inherited genetic variation – one that may impact immune response. The way that particular gene is expressed can be altered via the epigenome – a layer of chemical tags that sits on top of your DNA.
When environmental triggers – such as toxic chemicals, infections or other physical traumas, intestinal dysbiosis, or dietary factors– interact with the epigenome, they have the ability to activate or deactivate parts of the genome through complex chemical reactions.
Further study on the epigenome is needed, however the field of epigenetics highlights the critical role our lifestyle plays in either generating or preventing disease.
3. HAVING AN AUTOIMMUNE DISEASE
When you already exhibit one autoimmune disease, you’re at risk to develop more.
An accumulation of three or more autoimmune conditions is called Multiple Autoimmune Syndrome (MAS), which is seen in roughly 25% of patients.
It is common for individuals with certain conditions like celiac disease, rheumatoid arthritis, multiple sclerosis, Hashimoto’s, or Sjogren’s to exhibit MAS. The reason is unknown, but it is likely due to a combination of genetics and environmental factors.
4. OBESITY
Given that roughly 35% of the global population and 72% of adults in the U.S. are overweight or obese, it is critical that we recognize the relationship between obesity and other chronic conditions like autoimmune disease.
Excess weight is associated with over ten autoimmune diseases and may be implicated in others. It has been found to increase the risk of developing autoimmune conditions like rheumatoid and psoriatic arthritis.
Fat – or adipose tissue – is involved in many physiological functions, including metabolism and immune system response. When adipose tissue accumulates and becomes dysfunctional, it can lead to increased or dysregulated secretion of compounds called adipokines. In this case, these bioactive substances tend to be pro-inflammatory and significantly alter immune system function.
In other words, obesity sends the body into a chronic state of low-grade inflammation and can threaten an otherwise healthy immune response.
Research in this area is ongoing, but we are discovering that these factors (and potentially others, like alteration of the gut microbiota and intestinal dysbiosis) can lead to organ damage, metabolic syndrome, and autoimmune conditions.
5. SMOKING AND EXPOSURE TO TOXIC AGENTS
It is widely known that smoking cigarettes is not a healthy practice and can lead to cancer. Now, researchers are discovering that smoking is a risk factor in more than just respiratory conditions.
Smoking has been linked to rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, and other autoimmune diseases.
Why? When you burn tobacco, thousands of chemicals are produced – some of which are known to be toxic. Inhaling that smoke impacts the immune system through various complex interactions, including inflammatory responses, immune suppression, dysregulation of cytokines (signaling molecules involved in autoimmunity), and the development of autoantibodies.
Exposure to other toxins like air pollutants, crystalline silica, ultraviolet radiation, or organic solvents are also associated with the development of autoimmune diseases like multiple sclerosis.
Moreover, a genetic predisposition to autoimmunity further increases your risk. Many toxic agents have the ability to alter gene expression. In a nutshell, they can activate an otherwise repressed gene or deactivate an active one, leading to disease.
6. CERTAIN MEDICATIONS
Many people take pharmaceuticals on a daily basis to decrease blood pressure, manage depression and anxiety, or balance cholesterol levels. And it’s common knowledge that these drugs have potential side effects.
We’re discovering that in some cases, these side effects involve immune system function, and will trigger autoimmune reactions.
Certain blood pressure medications, statins, and antibiotics can trigger drug-induced autoimmune conditions like lupus or autoimmune hepatitis.
7. INFECTIONS
Early exposure to certain infections increases your susceptibility to autoimmune disease.
The presence of Epstein Barr Virus (EBV), which tends to present as a mild illness in childhood and then turn dormant, is associated with systemic lupus erythematosus, rheumatoid arthritis, and Sjogren’s syndrome.
Another infectious microorganism – a bacteria called Group A Streptococcus – can trigger heart, joint, and brain-related autoimmune disease including acute rheumatic fever and rheumatic heart disease.
These viruses interact with your genetics through a variety of mechanisms. In short, they can turn on certain genes that impact the immune system’s ability to differentiate between self and non-self, triggering an autoimmune reaction.
SARS-CoV-2 virus is associated with autoimmune disease in various ways, although researchers are still investigating the relationship. COVID-19 infection has been reported to trigger cases of Guillain-Barre syndrome, antiphospholipid syndrome, lupus, and other diseases. - Source: medicalnewsdaily.com
STATS:
Common autoimmune disease testing:
• Antinuclear antibodies (ANA)
• Autoantibodies
• Secretory IgA antibodies
• Thyroid function
• Inflammation
• Organ function
Did you know?
Covid-19
Infectious microorganisms such as SARS-CoV-2 can turn on certain genes and impact the immune system’s ability to differentiate between self and non-self, thus triggering an autoimmune reaction.
Health tip
Eat a nutrient-dense diet and limit processed foods
Health precaution tip
Keep up with the latest information about your medications
Talk with your doctor about specific ways you can reduce your personal risk.






Comments
Namibian Sun
No comments have been left on this article